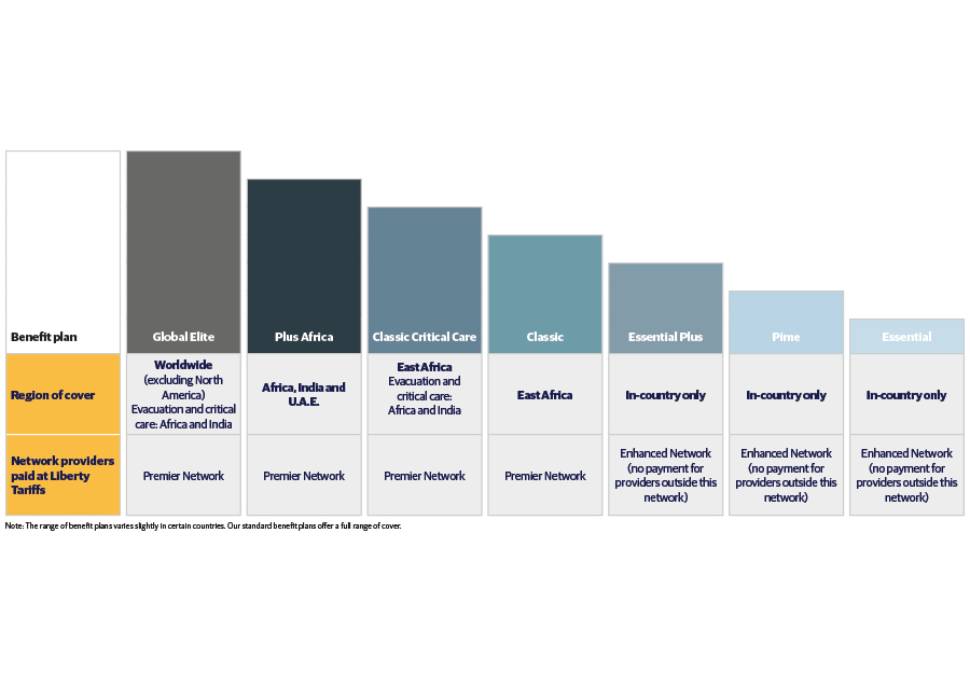
Range of Liberty Health Cover plans
We offer a wide range of Liberty health insurance plans with different levels of cover. The plans differ by region of cover, the level of limits and size of provider network that members enjoy.
The Benefits

- Day-to-day benefits
- Psychological wellbeing benefits
- Chronic conditions benefit for over 100 conditions like diabetes, high blood pressure, asthma etc.
- Hospital and major disease benefits for critical health events
- International health insurance benefits on select plans.
View our Brochure
To assist you to get a better understanding and explanation of all the policy benefits, download our brochure here.
Contact Details
Here are support numbers you can use
Frequently Asked Questions
As a valued member, please download and read your Liberty Health Cover Membership Guide to understand how your benefits work. Click here and scroll down to the Health section to find your Membership Guide.
The Member Guide explains the benefits under your key categories of cover, and:
- What to do in an emergency
- How to update your membership
- How to get pre-authorisation for hospitalisation and specialised treatment
- How to join our chronic and oncology programmes
- How to submit a claim for reimbursement
- What type of treatment and medication is excluded from cover
You need it for the following to ensure your claims are paid against the correct benefits:
- Hospitalisation (elective or planned and non-elective or emergency admissions)
- Cancer treatment (inpatient and outpatient)
- Renal (kidney) dialysis (inpatient and outpatient)
- Specialised radiology (inpatient and outpatient)
- Emergency evacuation (in-country and international)
- Chronic medicines
- An appliance or a prosthesis
- Organ transplants
- Ambulance services (air and road)
- Specialised dentistry
Email us at operationsuganda@libertyhealth.net or call us on +256 414 233 794 or +256 779 558 733 at least 48 hours (2 business days) before a planned treatment or admission.
For an emergency admission, a friend or family member can contact us within 48 working hours of the event. Or, if it is a weekend or public holiday, the next working day.
Complete and submit the relevant pre-authorisation form. You can download it from the Forms and Documents section of the website under the Health section.
Information we need:
- Patient’s full name, policy number and date of birth
- Treating healthcare provider details: full name and practice number
- Hospital details: full name of hospital and practice number
- Reason for admission or emergency visit (medical and/or surgical condition)
- Date of admission and proposed date of the procedure
- Additional supporting documents where required
- When a procedure is done out of hospital, for example, MRI (out-patient radiology), you need to supply the healthcare provider’s name and practice number
We will email you the outcome within 48 hours (2 business days) of your request. You will also receive a pre-authorisation number when we approve a request.
Your provider must update us regularly on the level of care you need and the length of the hospital stay required. Payment will be made based on the pre-authorisation and available benefits.
You or your healthcare provider can submit claims to our administration office by email or post at:
Email: operationsuganda@libertyhealth.net
OR
Post:
Liberty Life Assurance Uganda Limited,
Madhvani Building,
Plot 99 -101, Buganda Road,
Kampala, Uganda
Information that must be clearly visible on the claim:
- Membership/policy number
- Patient’s name and surname
- Patient’s date of birth
- Diagnosis
- Date of service (include admission & discharge dates for hospitalisation)
- A detailed description, per item, of the treatment or service received/provided (i.e. name of medicine, ward level)
- Quantity (i.e. 30 Disprin, 3 days in General Ward)
- Tariff code (if available)
- Amount charged per service or treatment (as per the contracted Tariff price list)
- Name of the treating healthcare professional
- Facility name (i.e. General Hospital, Africa Medical Clinic)
- Total charged (the sum of the individual amounts charged on the claim)
- Pre-authorisation number (if applicable)
- Proof of payment (receipt or proof of electronic (EFT) payment), in the case of a refund request for the principal member. The only document we will accept as proof of payment is a receipt or proof of electronic (EFT) payment. If the correct proof of payment is not attached, the account will be rejected.
- Signature of the insured person or principal member if the insured person is a minor
- Signature of the provider
- Date of the account and account reference number
For more information on how long payment takes or how often we send statements, please check your Membership Guide.
We pay for chronic medicines that are approved by our Chronic Disease Programme at 100% of cost, without co-payments, from your available benefits and according to the relevant medical and policy conditions.
Chronic conditions are conditions such as diabetes and high blood pressure that require medication and treatment for more than three (3) continuous months. Please check our Chronic Disease List in the next FAQ for a full list of conditions that we cover. Alternatively, check your Membership Guide.
If you are diagnosed with a chronic condition, together with your doctor or specialist, please complete and submit a Chronic Medicine Application Form to your in-country office.
Once you are registered on the Chronic Disease Programme, you will have access to:
- The Chronic Medicine Benefit to cover the cost of your chronic medication, and
- Additional benefits for related pathology, consultations and basic radiology.
By registering with the Programme, you can prevent claims for your chronic condition being paid from your Day-to-day benefits. Registration on the Programme is not automatic, so please apply as soon as possible.
Please contact us if there are any changes to your treatment.
Please contact your in-country office to pre-authorise any changes to your chronic treatment or medication. This will help us to ensure that claims are paid from your available benefits.
We cover pre-authorised treatment for the following chronic conditions from the chronic medicine benefit provided you register with the Chronic Disease Programme and your treatment has been pre-authorised together with your treating provider by our team:
- Acne
- Addison’s disease
- Allergic rhinitis
- Alzheimer’s disease
- Anaemia
- Ankylosing spondylitis
- Anorexia nervosa
- Arrythmias and conduction disorders
- Asthma
- Attention deficit hyperactivity disorder (ADHD)
- Barrett’s oesophagitis
- Benign prostatic hypertrophy
- Bipolar mood disorder
- Bronchiectasis
- Bulimia nervosa
- Cardiac failure
- Cardiomyopathy
- Chronic obstructive pulmonary disorder (COPD)
- Chronic renal disease
- Conn’s syndrome
- Cor pulmonale
- Coronary artery disease/Ischemic heart disease
- Crohn’s disease
- Cushing’s disease
- Cystic fibrosis
- Deep vein thrombosis
- Depression
- Dermatitis/eczema
- Dermatomyositis
- Diabetes insipidus
- Diabetes mellitus type 1
- Diabetes mellitus type 2
- Diverticular disease
- Dysrhythmias
- Dystonia
- Endometriosis
- Epilepsy
- Gastro-oesophageal reflux disorder (GORD)
- Generalised anxiety disorder (GAD)
- Glaucoma
- Gout
- Haemophilia
- Hepatitis B
- Hepatitis C
- HIV/AIDS
- Hyperlipidaemia
- Hyperparathyroidism
- Hypertension
- Hyperthyroidism
- Hypoparathyroidism
- Hypopituitarism
- Hypothyroidism
- Malabsorption syndrome
- Male hypogonadism
- Meniere’s disease
- Menopausal and perimenopausal disorders
- Menorrhagia
- Motor neuron disease
- Multiple sclerosis
- Muscular dystrophy
- Myasthenia gravis
- Neuropathy
- Obsessive compulsive disorder (OCD)
- Osteoarthritis
- Osteoporosis
- Paget’s disease
- Paralytic syndromes and associated complications
- Parkinson’s disease
- Pemphigus
- Polyarteritis nodosa
- Polycystic ovarian syndrome
- Polymyalgia rheumatica
- Post-traumatic stress disorders
- Primary/idiopathic thrombocytopaenic purpura
- Psoriasis
- Psoriatic arthritis
- Pulmonary interstitial fibrosis
- Rheumatoid arthritis
- Rosacae
- Sarcoidosis
- Schizophrenia
- Scleroderma and systemic sclerosis
- Sicca syndrome
- Stroke
- Systemic lupus erythromatosus
- Thrombosis and embolism
- Tourette’s syndrome
- Transient ischaemic attacks
- Trigeminal neuralgia
- Tuberculosis
- Ulcerative colitis
- Urinary incontinence
- Urinary tract infection (chronic)
- Valvular heart disease
- Zollinger-ellison syndrome
Please visit the Forms and Documents page and scroll down to the Health section to find important membership, banking details and pre-authorsation forms, as well as benefit tables, membership guides, policy conditions and so on.


